 | |
| Background Radiation Sources |
How much radiation am I exposed to with x-rays at the dentist? Are x-rays necessary? An exam with 4 bitewings is about 0.005 mSv, less than one day's worth from natural background radiation, and is the same exposure amount from an airplane flight of ~2 hours. Such are legitimate questions patients may ask when they visit the dentist for their annual checkups and cleanings.
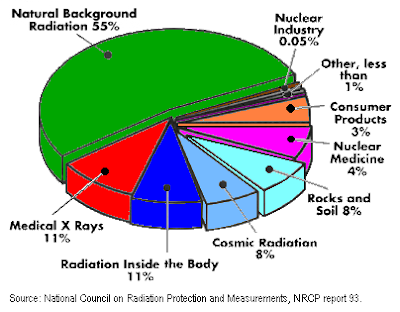
On should consider that EVERYONE is exposed to radiation EVERYDAY. The amount exposed depends on where you live, how much time you spend outdoors, and even your occupation. By far radon is the largest contributor to background radiation. Over 50% of daily radiation exposure comes from radon (radon has no smell, no odor, no taste, no color, and is present in your house due to trapped pressure from the rocks and soil underneath houses and buildings). Other sources of daily radiation include the sun,daily consumables, some tests required at the hospital, external rocks and soils, and various internal elements in the human body. In comparison, dental x-rays amount to less than 0.1% of the annual radiation exposure.
- WHY ARE X-RAYS NECESSARY AT THE DENTAL OFFICE?
- Diagnose cavities between your teeth
- Check for cavities underneath crowns and fillings
- Check for bone loss and periodontal disease
- Make sure your hard tissue and soft tissue adjacent to the oral and maxillofacial structures are normal
- Check the position of your wisdom teeth and evaluate for possible tooth extraction
- Examine how your children's baby teeth are erupting
- Orthodontically evaluate the positioning of your teeth and determine if braces and/or invisalign are options to correct any occlusal misalignment
- Check for missing permanent teeth
- Evaluate pathology, swelling, cancer, and many others...
From your gentle dentist in Bellevue and Redmond,
Peter Chien, DMD, MPH
www.bellevuefamilydentistry.com
(425) 614-1600






